What is a retinal vein occlusion?
A retinal vein occlusion occurs when a vein in the eye’s retina is blocked. The retina is the layer of light-sensing cells lining the back of your eye. It converts light rays into signals which are sent through the optic nerve to your brain where they are recognized as images.
A blocked vein damages the blood vessels of the retina. Hemorrhages (bleeding) and leakage of fluid occur from the areas of blocked blood vessels.
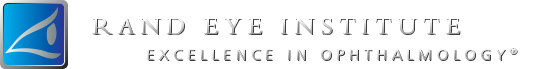
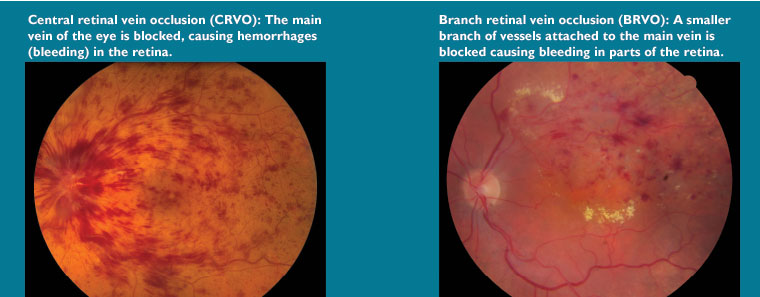
There are two different types of retinal vein occlusion:
- Central retinal vein occlusion (CRVO): when the main vein of the eye (located at the optic nerve) becomes blocked.
- Branch retinal vein occlusion (BRVO): when one of the smaller branches of vessels attached to the main vein becomes blocked
Who is at risk for a retinal vein occlusion?
Certain illnesses increase your risk for developing retinal vein occlusion including:
- Diabetes
- Glaucoma
- High blood pressure
- Age-related vascular (blood vessel) disease
- Blood disorders
If a branch retinal vein occlusion occurs in one eye, there is an increased chance (about 10 percent) that a branch or central vein occlusion will occur in the other eye in the future.
What are the complications and symptoms of retinal vein occlusion?
Macular edema: If blood and fluid leak into the central part of the retina called the macula, swelling of the macula occurs (called macular edema). The macula is the part of your retina responsible for your fine detail vision. It is what allows you to read small print, thread a needle, and read street signs. Macular edema causes blurred vision, decreased vision or both.
Abnormal blood vessel growth (neovascularization):
Retinal vein occlusion can cause abnormal vessels to begin to grow on the retina. These new vessels are very fragile and may bleed or leak fluid into the vitreous, the gel-like substance that fills the center of the eye. Small spots or clouds in your field of vision called floaters can appear. In more advanced cases of neovascularization the abnormal blood vessels may actually cause the retina to detach from the back of the eye.
Pain in the eye:
In severe cases of CRVO a blocked vein causes abnormal blood vessel growth on the iris and drainage channels in the front of the eye leading to painful pressure in the eye (neovascular glaucoma).
If complications from retinal vein occlusion are not treated, irreversible blindness may occur.
How is retinal vein occlusion detected?
Your ophthalmologist detects retinal vein occlusions by examining the retina with an instrument called an ophthalmoscope. The ophthalmologist may also perform fluorescein angiography, a procedure that takes special photographs of the eye, in order to further investigate the blood vessels in your eye.
How is retinal vein occlusion treated?
There is no known cure for retinal vein occlusion, though in some cases intraocular injections, laser surgery, or an operation may be used to reduce the macular edema and stabilize or improve vision. In severe CRVO, laser surgery is used to prevent or treat the abnormal blood vessel growth that can lead to glaucoma or bleeding. In some cases surgery may be necessary.
You may be able to prevent retinal vein occlusion from occurring again by properly managing any health conditions that contribute to this eye problem (such as diabetes, glaucoma, or high blood pressure).
If you have been diagnosed with retinal vein occlusion it is important to discuss and understand all your options.