What is uveitis?
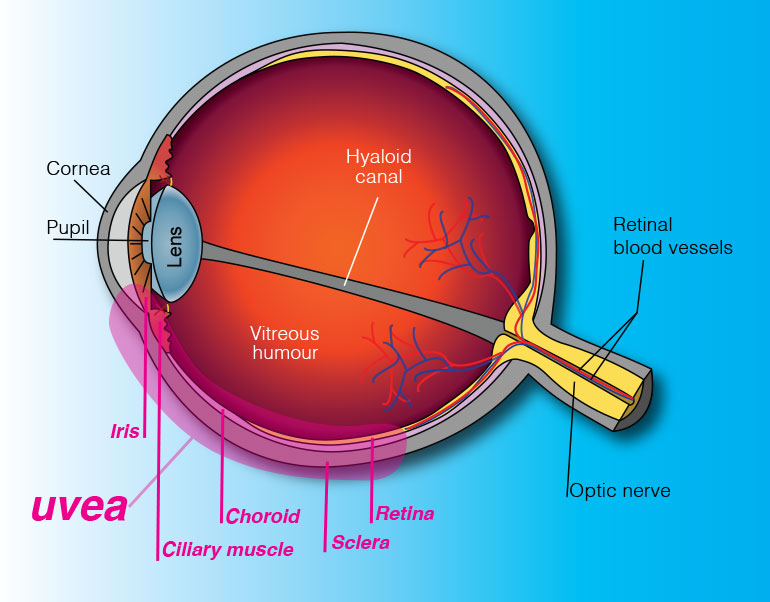
The eye is shaped much like a tennis ball, with three different layers of tissue surrounding the central gel-filled cavity.
The innermost layer is the retina, which senses light and helps to send images to your brain. The middle layer between the sclera and retina is called the uvea. The outermost layer is the sclera, the strong white wall of the eye. Uveitis (pronounced you-vee-EYE-tis) is inflammation of the uvea.
What is the importance of the uvea?
The uvea contains many blood vessels, veins, arteries and capillaries, that carry blood to and from the eye. Since the uvea nourishes many important parts of the eye (such as the retina), inflammation of the uvea can damage your sight.
What are the symptoms of uveitis?
- Light sensitivity
- Blurred vision
- Pain
- Floaters
- Redness of the eye
Uveitis may develop suddenly, with redness and pain, or with a painless blurring of your vision.
A case of simple “red eye” may in fact be a serious problem of uveitis. If your eye becomes red or painful, you should be examined and treated by an ophthalmologist (Eye MD).
What may cause uveitis?
- A virus, such as herpes simplex
- A fungus, such as histoplasmosis
- A parasite, such as toxoplasmosis
- Related disease in other parts of the body, such as arthritis, gastrointestinal disease or collagen vascular disease such as lupus
- A result of injury to the eye
If you smoke, stop. Studies have shown that smoking contributes to the likelihood of developing uveitis. In most cases of uveitis, the cause of the disease remains unknown.
How is uveitis diagnosed?
A careful eye examination by an ophthalmologist is extremely important when symptoms occur. Inflammation inside the eye can permanently affect sight or even lead to blindness if it is not treated.
Your ophthalmologist will examine the inside of your eye. He or she may order blood tests, skin tests or x-rays to help make the diagnosis.
Since uveitis can be associated with disease in other parts of the body, your ophthalmologist will want to know about your overall health. He or she may want to consult with your primary care physician or other medical specialists.
Are there different kinds of uveitis?
There are different types of uveitis, depending on which part of the eye is affected.
When the uvea is inflamed near the front of the eye in the iris, it is called iritis. Iritis has a sudden onset and may last six to eight weeks.
If the uvea is inflamed in the middle of the eye, it is called pars planitis (or intermediate uveitis). Episodes of pars planitis can last a few weeks or many years. The disease goes through cycles of getting better, then worse.
An inflammation in the back of the eye is called posterior uveitis. Posterior uveitis can develop slowly and often lasts for many years
How is uveitis treated?
Uveitis is a serious eye condition that may scar the eye. It needs to be treated as soon as possible.
Eyedrops, especially corticosteroids and pupil dilators, can reduce inflammation and pain. For more severe inflammation, oral medication or injections may be necessary.
Uveitis can be associated with these complications:
Glaucoma (increased pressure in the eye)
Cataract (clouding of the eye’s natural lens)
Neovascularization (growth of new, abnormal blood vessels)
Damage to the retina, including retinal detachment
These complications may also need treatment with eyedrops, conventional surgery or laser surgery.
If you have a “red eye” that does not clear up quickly, contact your ophthalmologist.