SOL Shine Recognition Award
During our meeting in Orlando, our clinical trial department @randeyeinstitute Carl Danzig, MD and Damian Stega, received the SOL Shine Recognition Award as a center of excellence for the management of WET MACULAR DEGENERATION patients in the SOL-1 and SOL-R clinical trials. We are extremely proud of our clinical trial team and forever grateful for the trust our patients have bestowed upon us. Thank you @oculartherapeutix for this honor! hashtag#randeyeinstitute
Clinical Trials Study investigates gene therapy for vision condition
Rand Eye Institute Director of Vitreo-Retinal Services Dr. Carl Danzig is the first in South Florida to administer an investigational gene therapy for people with dry age-related macular degeneration, commonly known as AMD.
The clinical trial, called Horizon, involves a single, one-time injection under the retina at the back of the eye to deliver this gene therapy.
“This is different than wet macular degeneration, which people know about, that takes place in the office. This is in the operating room, where we enter the eyeball and we go under the retina with a very tiny needle and we inject some gene therapy, and what this does, it provides instructions for your own cells to produce a natural regulatory protein that you already have and basically upregulate that — you make that more and therefore, hopefully, fight the progression of this disease,” Danzig said.
Click the link below to watch the full interview as seen on Local 10 HealthCAST with Kristi Krueger.
https://www.local10.com/health/2022/02/17/study-investigates-gene-therapy-for-vision-condition/
What is iDesign Technology?
Laser Vision correction has come a long way since its inception. The parameters of corrections that can be treated today were just a dream a few years ago. A good correction has become an exact personalized treatment for each eye. At Rand Eye Institute, we are dedicated to being up to date with the latest FDA-approved technology. This is the reason why we utilize our Star S4 IR Excimer Laser System and iDesign 2.11 Advanced Wavescan Studio System – the finest technology in laser vision correction.Up until a few years ago, an ophthalmologist used your eyeglass prescription to determine your treatment. iDesign technology has revolutionized laser vision correction by providing a detailed map of the surface of the eye plus information on how well your cornea and lens refract light.

The iDesign system scans your cornea to provide information on the eye’s low order aberrations (myopia, hyperopia, and astigmatism), and high order aberrations (personal characteristics of an eye that cause halos, glare, and poor night vision). Consequently, the surgeon, now, has the full spectrum of refractive errors that need to be corrected to provide excellent visual outcomes. The iDesign system and technology are called wavefront integrated vision correction. This system collects 1,200 data points of your eye. Hence, making the treatment 25 times more accurate than just checking your vision and glass prescription.
The detailed iDesign map is then sent to the Star S4 IR Excimer Laser System. This detailed map provides all the information for the excimer laser to know where and how to sculpt the cornea for best visual outcomes. No two eyes are the same. Tiny personal characteristics in your cornea (like your fingerprint) create visual errors. These characteristics can only be measured with the iDesign system.
Our mission at Rand Eye Institute is to provide our patients with the best possible visual outcome. iDesign technology allows us to achieve an even higher degree of vision.
Love your vision for years to come! Call Rand Eye Institute at 954-782-1700 for your complimentary LASEK consultation.
May is Healthy Vision Month

What are the most important tips to maintaining a healthy vision? We asked our doctors and came up with a simple list that everybody can follow. Your eyes are the window to the world. You get only one set so please be kind to them, so they can take care of and protect you!
- An Annual Eye exam.
Many people believe that if you do not have any issues with your eyes, you do not need to have them checked. Your eye physician needs to know how your eyes are when you are healthy and then compare test results when an issue arises. In ophthalmology, if a condition is caught early, chances are best at treating it or stopping its progression. Many common eye diseases like glaucoma, diabetic eye disease, and macular degeneration often do not provide warning signs. No one can afford to be lazy with their eyes! - Eat a balanced diet.
Eating a balanced diet will keep you and your eyes healthy. Nutrients such as Omega-3 fatty acids, zinc, and Vitamin C provide extra nourishment and vision protection. A diet rich in fruits and vegetables, particularly dark leafy greens such as spinach, kale, or collard greens, as well as foods rich in Omega-3 fatty acids like salmon, tuna, eggs, and nuts are important to maintaining a healthy vision. - Do not Smoke!
Smoking is as bad for your eyes as it is for your lungs and the rest of your body. Studies have linked smoking with the development of age-related macular degeneration and optic nerve damage. - Exercise
When a person exercises, the circulation improves in the body and thus the toxins are released. For the entire body to be healthy, a person needs good circulation. Make your exercise fun. Find an activity that makes you smile! Enjoy it! - Wear Sunglasses.
We are lucky to live in sunny Florida. We love sunny skies and the beautiful weather. However, please do not forget to protect your eyes! Choose sunglasses that block 90% of both UVA and UVB rays. For long walks, wear a hat to provide extra protection. - Wear Protective Eyewear.
Wear protective eyewear when playing sports, working on your hobby, gardening, etc. Also, remember to wear protection at work if it’s deemed necessary to your profession. - Get informed about your family’s eye health history.
Ask your relatives about their eye conditions if any. Some conditions are hereditary. This information will help determine if you are at a higher risk for the development of an eye disease or condition. Remember most eye conditions, if caught early, can be treated or slow down their progression. - Give your eyes a rest.
Try the 20-20-20 rule! Every 20 minutes look away about 20 feet in front of you for 20 seconds. This exercise helps with eye strain.
These tips are not hard to follow. One just needs to make a conscious effort to be kind to their eyes. If you have any questions, please call your eye physician for more detailed information. Rand Eye Institute is just a call away if you need assistance our ophthalmologists are on-call 24/7. Your eyes are important to us!
April is Women’s Eye Health Month and Sports Eye Safety Awareness Month

The month of April reminds us of two very important topics: Women’s Eye Health and Sports Eye Safety month. Rand Eye Institute is very aware of the importance of these two important topics as we see the daily consequences, they cause our patients. In Women’s Eyes Health prevention is key. This goes back to the importance of annual eye exams. On the other hand, for Sports Safety, protection is the name of the game. Keywords for April are Prevention and Protection.
The Prevent Blindness organization states that women have higher rates of eye diseases such as cataracts, glaucoma, and age-related macular degeneration than men. Women also tend to have a higher rate of dry eyes and often deal with vision changes due to hormonal changes, pregnancy, and menopause. It is important to note that women are usually the caregivers for the entire family, hence, the further importance of their eyesight. The National Eye Institute stated that women deal with greater instances of eye disorders because they tend to live longer lives than men. Therefore, women are more likely to undergo cancer treatments which affect their vision. Medications, Hormonal treatments, hormonal imbalances can produce vision changes. Annual Eye exams will detect most conditions which, if caught early, can be treated or controlled.
Sports Eye Safety is another important topic to reflect on. Accidents will happen when playing sports, but if you are protected, you will not get injured. Eye Protection should fit comfortably and protect eyes without compromising on your athletic performance. This is true especially when it comes to the health of your eyes.
Here are some tips when buying sports protection:
- Consult an eye care professional to get the best eye protection for your sports, hobbies, and lifestyle
- Ask your eye doctor to fit you with prescription eye protection if you need glasses
- Please remember that protection needs to be cushioned and well fitted to your face so that it does not cut the skin in case of contact with an object.
- Make sure the purchased eye protection fits well. Consult with an eye professional.
We are back to our two keywords. Prevention by attending your annual eye exams is very important for everybody but especially for women. And protection to prevent any injury. You can have fun and be fit without the fear of compromising your vision. Have a great and healthy month of April! Call 954-782-1700 for your annual eye exam.
Workplace Eye Wellness – Tips to Consider

Workplace Eye Wellness Month
Tips to Consider
According to the CDC, more than 2,000 US workers sustain eye injuries every day. We must educate people on how to address these preventable injuries. The first step is to have the workplace, whether it is a factory, an office, or a park, engage in the education and supervision of the safety of their staff. The Occupational Safety and Health Administration (OSHA) requires employers to ensure the safety of all their employees. Eye and face protection must be provided whenever a potential exposure to chemical, radiological, or mechanical irritants are present.
Safety eyewear includes:
- Non-prescription / prescription safety glasses
- Face Shields
- Welding helmets
- Full face respirators
Eye wellness must also be taken into consideration in the office environment. Too much screen time and not enough breaks can lead to headaches, neck pains, back strain, and dry eyes. When we stare at a screen for an extended period, we are not blinking as often and thus the eyes are not getting lubricated. Lack of lubrication leads to dry eye symptoms a condition that can be quite bothersome and painful.
Here are some tips on ways to protect your eyes from dry eye syndrome:
- Remember the 20-20-20 rule. Every 20 minutes look at an object 20 feet away for 20 seconds.
- Do not forget to blink
- Use artificial tears
- Drink water
- Schedule regular eye appointments with your eye physician.
- If you already have dry eyes, Rand Eye Institute offers special dry eye appointments on Tuesdays with Dr. Allison Rand.
Most eye conditions can be treated if caught early. An eye physician can prescribe and provide the tools to treat dry eye syndrome. Please do not procrastinate on scheduling your next eye appointment. Your vision is a precious gift, take care of it!
Stargardt’s Macular Degeneration
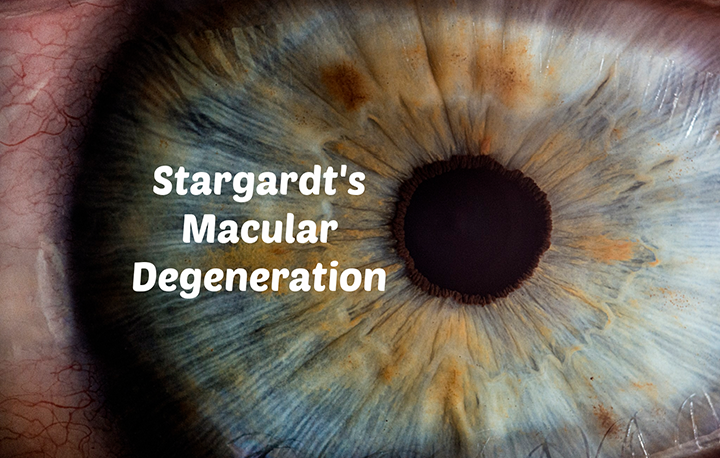
Stargardt’s disease is an inherited disorder of the retina. This disease starts to develop visual changes in patients in their childhood or teenage years. The changes are gradual but constant until their vision is decreased approximately to 20/200 or worse uncorrected. This condition is also called Stargardt’s macular dystrophy, juvenile macular degeneration, or fundus flavimaculatus. This disease damages or degenerates the macula, which is in the retina. The macula is the area in the eye that delivers sharp straight-ahead vision.
Patients with Stargardt’s experiences a slow and constant central vision loss, hence, becoming sensitive to bright lights. The retina contains light-sensing cells called photoreceptors. These are called rods and cones. Both rods and cones photoreceptors gradually die due to this disease.
As we mentioned earlier, this disease is inherited in most instances due to a mutation in a gene called ABCA4. The ABCA4 gene created a protein that clears Vitamin A byproducts inside the photoreceptors. Due to the cells not being cleansed, the cells become full of fatty substances and consequently the cell dies. This degeneration starts to happen around the macula which is the reason why patients start losing their central vision.
To diagnose Stragardt’s disease, an eye physician needs to do a thorough and complete eye exam.
The following tests are recommended:
- Slit eye exam. An eye physician will see the fatty deposit in the macular under the microscope if Stargardt’s is present
- Visual field testing to determine the areas and progression of the disease
- Color testing determine if the patient is becoming color blind
- A fundus photo which is a detailed picture of the retina
- An electroretinography (ERG) measures the response of cones and rods to light
- Optical Coherence Tomography (OCT) which is a light wave scanning device of the retina
Treatment Options
Unfortunately, there is no treatment for Stargardt’s. Patients are encouraged to wear dark sunglasses, not to smoke, and not to take Vitamin A supplements. Low vision aids are quite sophisticated right now and they can lend a lot of help by magnifying images or providing voice commands. Many Stargardts patients become visually disabled in their 20s which can take a significant emotional toll on the individual and their loved ones. Good medical eye care, counseling, and a supportive circle of friends and family are necessary to best confront this disease. There are multiple studies and research worldwide in the works addressing the degeneration of the macula. We look forward, with anticipation, to a new treatment in the medical field to aid all our patient’s with Stargardt’s and Macular Degeneration.
January is Glaucoma Awareness Month
Happy New Year! May 2021 bring us all health, peace and happiness.
Glaucoma is called “The Thief of Sight” because it occurs so gradually that you may not even be aware that you are experiencing vision loss due to glaucoma. Glaucoma occurs when pressure in the eye becomes higher than normal resulting in increased pressure on the optic nerve, pinching the blood vessels that carry blood to the retina and optic nerve.
While many people schedule a baseline screening every year or so, the BEST way to prevent glaucoma is with a comprehensive eye exam. Some people have a higher risk of developing glaucoma. If you are in any of these categories, please call us for a full eye exam:
- Relatives with glaucoma
- African, Asian, or Hispanic background
- Farsighted or nearsighted vision
- High eye pressure on previous exam
- Have diabetes, migraines, or high blood pressure
- Long term use of steroids
Glaucoma is one of the leading causes of blindness but it does not have to happen to you. Early testing and prevention are extremely important, especially since there is no known cure. For vision already lost due to glaucoma these are three procedures that can help to stop glaucoma in its tracks. If you are diagnosed with glaucoma, we can explain these options thoroughly and choose which is best suited for your condition. The goal of any treatment is to lower your eye pressure to a safe level.
- Prescription eye drops
- Laser glaucoma surgery
- Filtration surgery
Anyone can be at risk from glaucoma; everyone from babies to senior citizens can be at risk. Actually, 1 out of every 10,000 babies is born with glaucoma.
Here is the key: When glaucoma is diagnosed and treated adequately, vision can be preserved rarely ending in blindness, hence, the upmost importance of regular eye exams.
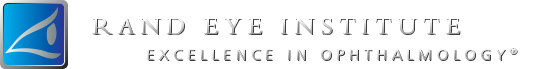
Dry Eyes Symptoms and Solutions with Lipiflow Treatments by Allison Rand, MD
Dry eye disease is more common than you might realize, with over 16 million Americans carrying the diagnosis. Many more patients may suffer from these symptoms without a diagnosis, and it has been suggested that one out of every two American adults may experience symptoms of dry eye. About one-third of all the patients I see have complaints that relate to dryness. These symptoms may include blurry vision, glare or light sensitivity, eye pain or foreign body sensation, itching, redness, burning, and tearing. Some patients may have difficulty wearing contact lenses, or notice eye fatigue after reading of watching television. These symptoms can occur in isolation or in any combination.
Most people think that dry eye is just not having enough tears. For some people this is true, but for most people, they might make enough water for the tears, but the tears do not stay on the eye long enough to coat the surface well. These individuals have tears that evaporate too quickly, or perhaps they have excessive tearing – meaning that the tears that are supposed to coat the eye instead run down the cheek. The reason for this is that there is another important part of a healthy tear film – the oil component – which helps the tears stick to the eye. These oils come from the Meibomian glands, tiny glands along the edge of the eyelids that release beads of oil with the force of each blink. If the Meibomian glands are inflamed from blepharitis or Meibomian Gland Dysfunction (MGD) – inflammation of the eyelids, the oil becomes thick and clogs the glands, preventing healthy oil from being released onto the surface of the eye.
Normal oil from the Meibomian glands is free flowing, like olive oil. Inflammation leads to oil that looks like toothpaste, or butter straight out of the refrigerator. When we treat blepharitis, we focus on warm compresses which help to “melt the butter” and improve the flow of oil out of the glands by using heat to liquefy the oil. This is used at least twice daily to maintain healthy Meibomian glands. At the Rand Eye Institute, we have the ability to use state of the art imaging technology called Lipiview, which can directly produce an image of the glands, so that our doctors and patients can see the health of the oil glands and decide on the appropriate treatment plan.
We are very excited to offer our patients who have MGD an additional therapy that is in addition to the traditional dry eye therapies that can be used at home. Lipiflow thermal pulsation technology is available at the Rand Eye Institute. Lipiflow uses a novel device to heat and massage the blocked glands in a 12-minute procedure as part of the exam in the doctor’s office. The system’s activators, which are single use and sterile, are placed on the eye, after numbing drops have been instilled. The procedure is not painful. Most patients say that it’s not only comfortable, but feels good, just like an extended warm compress in a spa-like environment. There is no downtime, and patients start to feel an improvement in symptoms within 4-6 weeks.
This procedure is perfect for patients who are symptomatic with dry eye disease, with Meibomian gland dysfunction that are doing all the correct treatments daily, but looking for something a little stronger to help with their symptoms. The analogy is that you may be brushing your teeth every day, but still want to go to the dentist for a deep cleaning. Lipiflow can be repeated as needed, and many patients choose to have touch up treatments once a year.
We are thrilled with how happy our patients are with the results of their Lipiflow treatments. Receiving proper treatment for dry eye can be life-changing. Please let us know if you are having dry eye symptoms so that we can select the right treatment plan for your individual needs. Give us a call for a dry eye consultation. Dry Eye relief is just a call away to Rand Eye Institute.
Image Enclosed from J&J.
National Children’s Eye Health & Safety Month
It’s August and while summer vacation is winding down, students and parents are preparing for another school year. This year, don’t forget to include on your back-to-school checklist an annual eye exam.
It is important to have your child’s eyes tested, because it can lead to greater success in the classroom since much of a child’s learning occurs visually.
Have you noticed any change in your child’s vision? Here are some signs and behaviors you can watch for that may indicate a child is struggling with his or her vision.

Is Your Child Doing Any of the Following?
- Rubs eyes frequently;
- Closes or covers one eye;
- Tilts head or thrusts head forward;
- Has trouble reading or doing other close-up work, or holds objects close to eyes to see;
- Blinks more than usual or seems cranky when doing close-up work; or
- Squints eyes or frowns.
Does Your Child Say Any of the Following?
- “I can’t see very well”
- After doing close-up work, your child says, “I feel dizzy,” or “I have a headache,”
- “Everything looks blurry,” or “I see double.”
It is recommended that your child have an annual eye exam to screen for any abnormal changes in vision or to confirm that all is well. Let’s start the new school year off with an “A” in vision!